DOI:
10.37988/1811-153X_2021_1_136Manufacturing and installation of a temporary conditionally removable orthopedic structure using the analog-digital method for one-stage implantation
Downloads
Abstract
When installing implants, a decision is not always made on the immediate loading of the orthopedic construction due to the fear of disrupting bone integration, which can lead to the loss of the implant, therefore, they resort to the delayed loading technique, which leads to a decrease in the quality of life. Objective. Manufacturing and installation after one-stage implantation of a conditionally removable prototype of an orthopedic structure previously used by the patient using the analog-digital method.Materials and methods.
The study and treatment of 26 patients who applied to the clinic «Vash Stomatolog» were carried out. To reduce the time of permanent prosthetics and improve the quality of life of patients after surgery, implantation, an analog-digital method of manufacturing temporary, conditionally removable, orthopedic structures was used using an intraoral optical scanner 3Shape Trios 3. The digital image in the form of an electronic STL file is sent to the Exocad program, where the operator makes changes and additions, including modeling the missing teeth. The digital images of the upper and lower jaws are saved in the program. Then a stereographic model of the jaws was made using the 3D-printing principle to visualize the clinical situation. On the multiunit platform, impression transfers are installed, a two-layer silicone impression is taken, which is sent to the dental laboratory for the manufacture of a plaster model and its fixation into the articulator. Temporary abutments are installed in implant analogs. The laboratory scanner has scanned the existing working model, which is fixed on the multiunit.
Results.
Thanks to the use of modern technological solutions, the shape of the future orthopedic structure for the patient was visualized, a temporary prosthesis was quickly manufactured and installed after the operation, in which the previous prototype was used.
Conclusion.
Immediate installation of a conditionally removable temporary orthopedic structure manufactured by the analog-digital method during a one-stage implantation leads to a reduction in the time of permanent prosthetics.
Key words:
optical scanner, temporary prosthetics, immediate loading, working model, primary implant stabilityFor Citation
Introduction
The development of digital dentistry makes it possible to shorten the period of provisional rehabilitation and the duration of permanent prosthetics for patients with partial or complete loss of teeth [1-6].
The digital planning of future work, as well as the use of modern surgical protocols make it possible to obtain high primary stability of the implant, leading to rapid regeneration of the bone tissue around the implant directly under the load of the prosthetic restoration.
The surgical protocol of one-stage implantation in patients with complete or partial loss of teeth is an atraumatic extraction with implants placed directly into the tooth socket or at an angle bypassing important anatomical formations, which makes it possible to obtain high primary stability of the implant of 35-45 N· cm2 [7-9].
Many specialists, when placing implants, having received a torque force of less than 35 N· cm2, do not always decide to load the prosthetic restoration immediately for fear of disrupting bone integration, which can lead to the loss of the implant, so they resort to the technique of delayed loading. During the period of implant integration, the rehabilitation of a patient with fixed restorations can be difficult and is often accompanied by the use of a removable prosthesis, which reduces the quality of life [10-15].
Removable prostheses used in patient rehabilitation, as a rule, do not meet the requirements of the old prosthetic design and are perceived as a foreign body [16-18]. Their use during the integration period of implants can lead to atrophy of the alveolar ridge, impairment of their integration into bone tissue, as well as to lengthening the duration of the final prosthetics.
Taking into account the above mentioned, it is necessary to obtain a prototype of the future prosthetic restoration in advance, using it subsequently for provisional rehabilitation of the patient until the period of final implant integration. One of these methods is the direct fabrication of a provisional prosthesis on implants using photocomposite and silicone key [19–25]. Intraoperative immediate prosthetics and placement of the prosthesis for 72 hours were used [26-29]. The technique made it possible, using the analog method, to make a cast frame in a dental laboratory and to install it in the mouth with special abutments, and to glue the finished conditionally removable prosthesis, quickly rehabilitating the patient.
The disadvantages of these techniques are: the time-consuming and labor-intensive work to fix the prosthesis after the implants are placed; the materials used require chemical polymerization for their hardening in the mouth during the placement of the restoration.
The use of digital technologies makes it possible to obtain a future prototype of a provisional prosthesis, having previously scanned old prosthetic restorations by the intraoral method, thus reducing the duration of patient rehabilitation at all stages of treatment [30].
The fabrication of a provisional conditionally removable restoration in a digital laboratory takes 3-4 hours and its placement in the mouth - up to 30 minutes.
The purpose of the work is to use an analog-digital method for fabricating a conditionally removable prototype of a prosthetic restoration previously used by a patient and to install it after a one-stage implantation.
Materials and methods
- Intraoral scanning. To create a future prosthetic restoration, it is necessary to obtain a digital image of the teeth, which will provide the ideal accuracy of the provisional restoration and speed up the patient's rehabilitation. Intraoral scanning by the 3Shape Trios 3 apparatus is a non-contact optical scanning of an object, which allows one to determine its geometric structure, where a light pulse is transformed into a 3D image and is saved in the form of an electronic file.
Using an optical sensor, an image is created, which is automatically converted into an open digital STL format to allow one to work in any program for modeling prosthetic restorations.
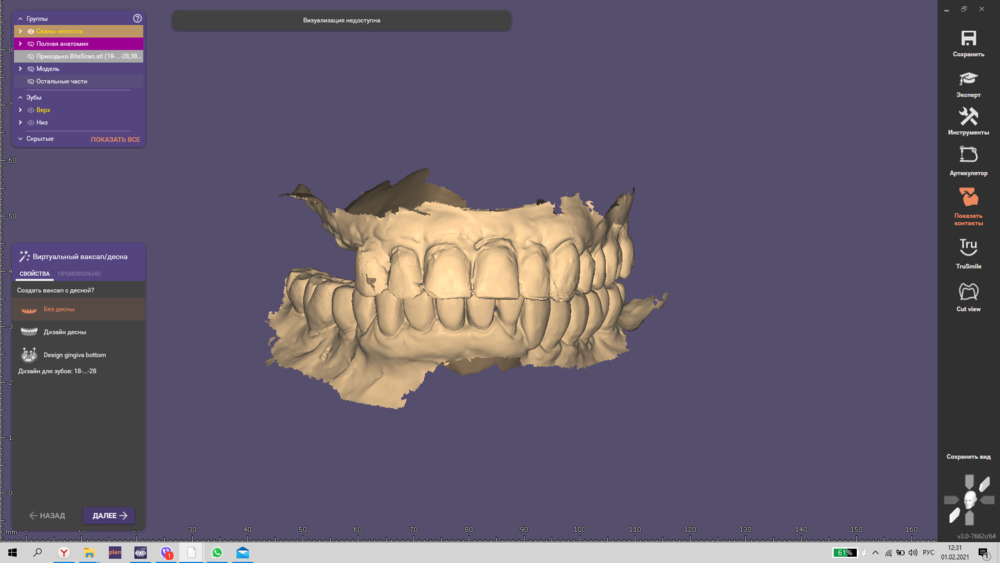
- Loading and modeling the restoration image. After the scanning stage, the Exocad program evaluates and additionally simulates the missing teeth, and, if necessary, corrects the shape of the old prosthetic restoration. In the 3Shape program, into which a computed tomography image in the DiCom format is preloaded, the virtual placement of the implants and the screwing angle relative to the image of the future prosthetic restoration are assessed.
- Stereolithography. Models for prosthetic treatment planning are fabricated in the Formlab3 apparatus using stereolithography technology, a laser sintering technique that makes it possible to digitally produce diagnostic demonstration models, individual mouthguards, prototypes of prosthetic restorations, and other three-dimensional objects. This technology allows one to quickly and accurately make an image of dentoalveolar models before and after treatment. After the implant is placed in the desired position, an analog stereographic model is created, which allows the specialist to see the final restoration.
- Thermal vacuumization. The UltraVac apparatus performs the necessary shaping of the thermoplastic material by crimping the dentoalveolar model with plastic. After the material has hardened, it is processed. The directing mouthguards are made in a similar manner.
- Laboratory scanning of the models was performed with a Ceramill Map600 laboratory 3D scanner (Amann Girrbach). The intelligent interface of the device allows one to move the scanned object in space and generate an STL file for further work in the simulation program.
- Milling was carried out in a five-axis Coritec350i laboratory machine, which makes it possible to use wet and dry processing of various materials, including PMMA. A special program calculates the milling mode by determining the speed and movement of the drill, as well as the type of the material and its characteristics. The open CAD/CAM system allows one to use electronic files from systems of other manufacturers.
Results and discussion
Using this technique, a study and treatment of 26 patients who applied to the clinic “Vas stomatolog” were carried out.
After planning and making a comprehensive treatment plan, the old prosthetic restoration is scanned using the 3Shape intraoral scanner. The position, shape, and aesthetics should satisfy the patient during the entire period of using the restoration. Next, scanning of the antagonist teeth and recording of the usual occlusion are performed.
The digital image in STL format is sent to the Exocad software, where the operator makes changes and additions, including modeling the missing teeth.
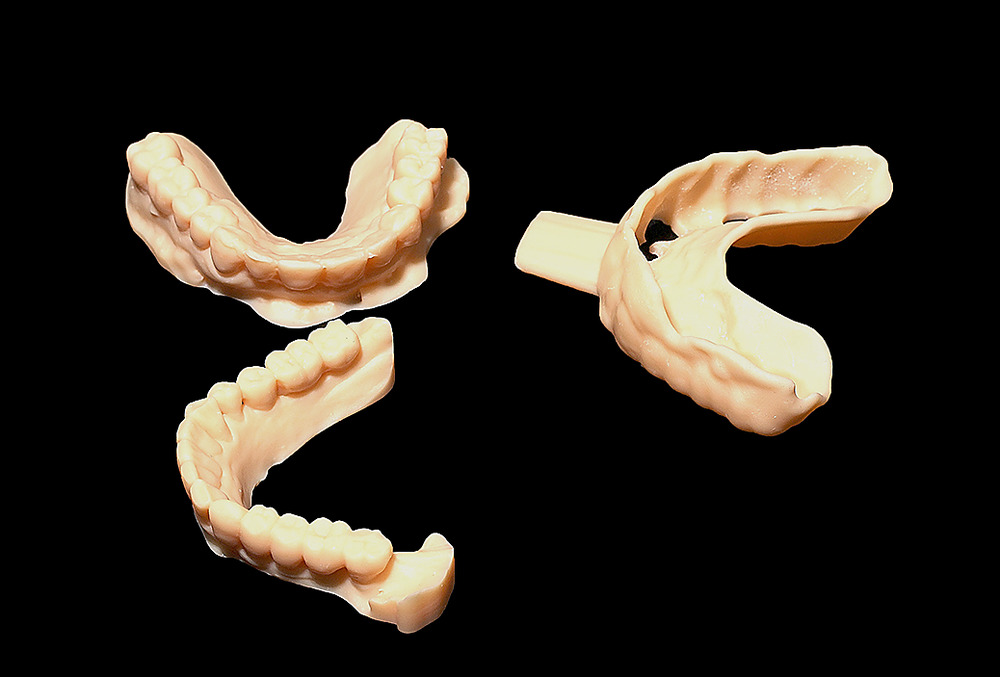
The digital image of the upper and lower jaws is stored in the program. Then a stereographic model of the jaws is made using the 3D printing principle to visualize the clinical situation. A template - a mouthguard - for planning the placement of implants in the correct position, which fully replicates the shape of the old restoration, as well as an individual spoon for taking a silicone impression from the implants during the surgery are preliminarily made according to the model (Figure 1).
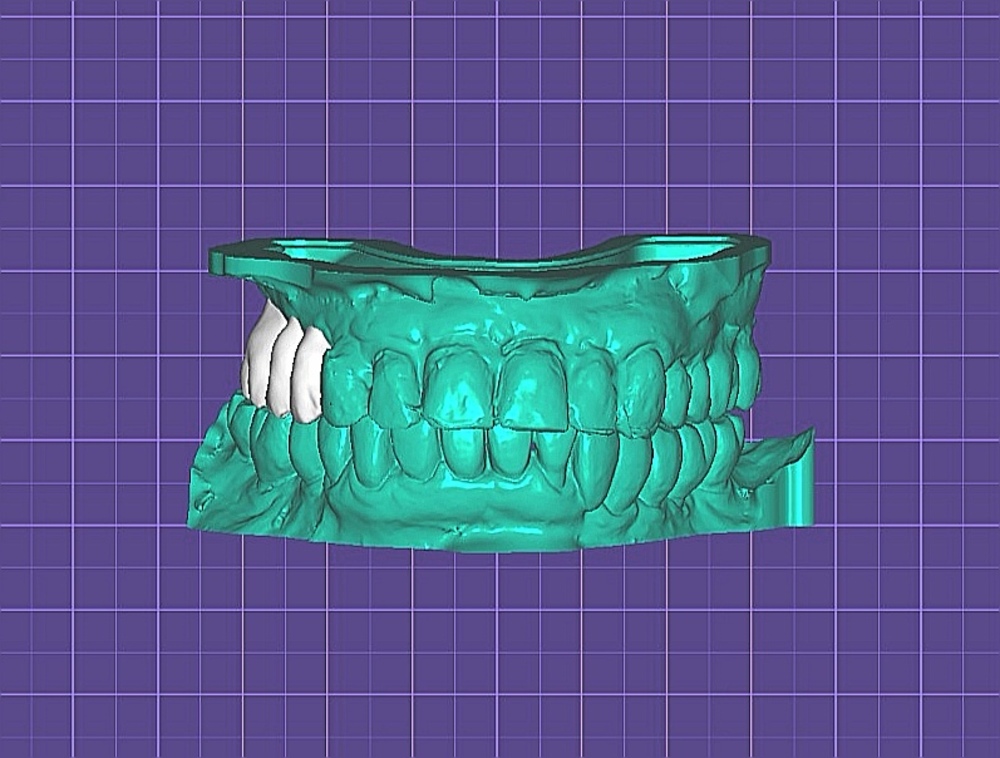
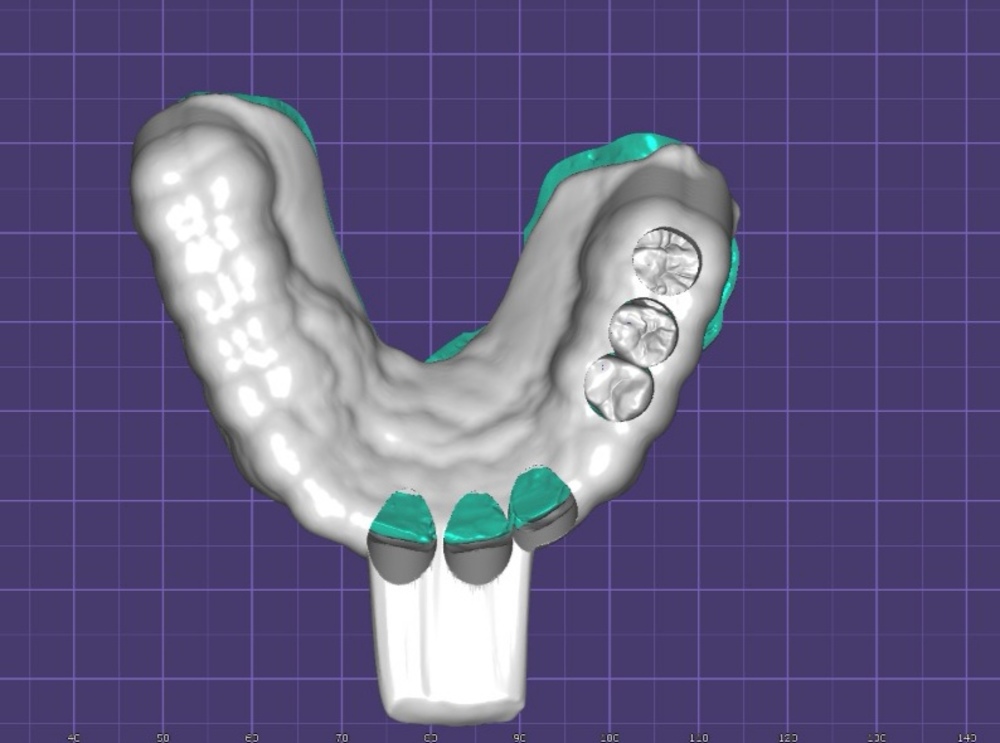
Figure 1. Stages of modeling: a — missing teeth; b — spoons for taking impression from the multiunit level
Surgery. After removing the old prosthetic restoration, atraumatic tooth extraction is performed. Before placing the implants, a template (mouthguard) is applied to plan the position of the prosthetic platforms with respect to the future provisional restoration.
Then, implants with a primary stability of at least 35 N· cm2 and an immersion depth of more than 2 mm relative to the alveolar ridge are installed in the extraction sockets. The overhanging edges of the cortical plate are removed with a special cutter, and prosthetic components (multiunit) are installed on the implants with a torque force of 15-30 N· cm2.
Some of the teeth whose position is selected without implants are retained to record the central jaw alignment. The patient is asked to close the teeth in their usual position; the bite is recorded with A-silicone; the teeth are atraumatically extracted, and the tooth sockets are augmented with a xenograft. Sutures are applied (Figure 2).

Figure 2. Completion of surgical phase — installation of multiunit
The next stage is prosthetics. The impression copings are placed on the multiunit platform and a two-layer silicone impression is taken using an individual spoon. The multiunit platform is closed with a protective shaping cap. The impression is sent to the dental laboratory to make a plaster cast and fix it in the articulator. The existing working model is scanned with a laboratory scanner, having previously placed provisional abutments in the implant analogs, as well as its position relative to the antagonists in the articulator (Figure 3).

A special program merges the saved image of the old prosthetic restoration with the image of the working model using several control points. Color areas appear in the program, showing the errors. Additionally, the shape and length of a new provisional restoration, which will be fixed on a multiunit, are modeled (Figure 4). After 2.5 hours, the milled PMMA restoration is ready.
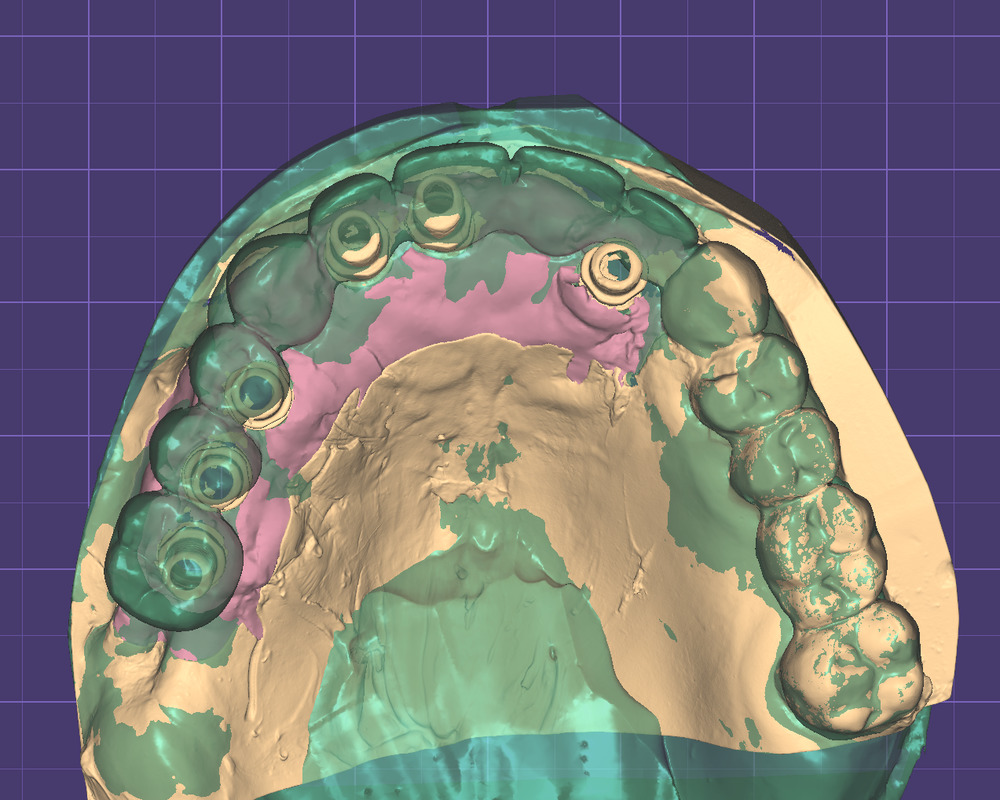

Figure 4. Stages of the work: a — merging the working model with the image of the old prosthetic restoration; b — provisional restoration after fabrication
Within 72 hours after the surgery, the restoration is fixed on prosthetic platforms with a load of 15 to 30 N· cm2. Occlusion control with antagonist teeth is performed.
Clinical case
Female patient N., 58 years old, complained of pain in the area of tooth 1.7 under the bridge construction (Figure 5).

Diagnosis: Partial secondary adentia, tooth loss due to accident, extraction, or local periodontal disease (K08.1). During emergency care, the bridge construction was segmented in the area of tooth 1.3 with the diagnosis “exacerbation of chronic periodontitis”; tooth 1.7 was extracted. One month after extraction, the patient developed mobility of teeth 1.3, 1.2, 1.1, and 2.1 under the old bridge construction. The bridge construction was partially removed; the rest of the prosthesis in the upper jaw was left intact for financial reasons. A decision was taken to make an atraumatic extraction of the upper jaw teeth in the area of teeth 1.3, 1.2, 1.1 and 2.1 with the immediate placement of implants and loading with a conditionally removable provisional restoration from the level of multiunit platforms.
At the planning stage, intraoral scanning of the old prosthetic restoration was performed with the fixation of its image in a special program (Figure 6). The missing teeth were modeled; stereographic models, a template (mouthguard) for planning, and an individual impression spoon for taking a silicone impression from the implants after surgery were made (Figure 7).
Before surgery, during the preparation stage, after removing the old prosthetic restoration, provisional crowns were made by direct method. Atraumatic extraction of teeth 1.3, 1.2, 1.1, and 2.1 was carried out, a template (mouth guard) was applied for the correct position of the multiunit platforms, and the implants were placed in the positions of teeth 1.4, 1.5, 1.6, 1.2, 1.1, and 2.2 (Figure 8). X-ray control was performed (Figure 9).

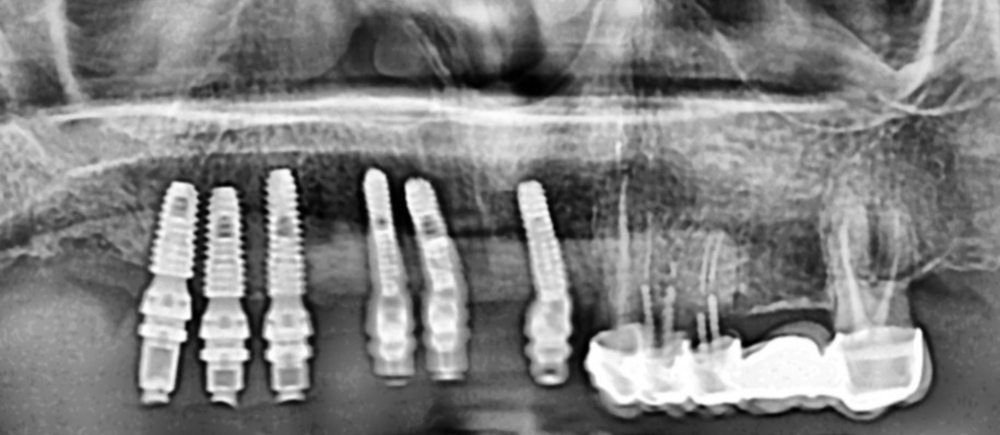
Then, the impression transfers were placed on the multiunit platforms, a two-layer silicone impression was taken using an individual spoon, and the bite was recorded with A-silicone. In the dental laboratory, a working model was made, on which the provisional abutments were placed and scanned (Figure 10).
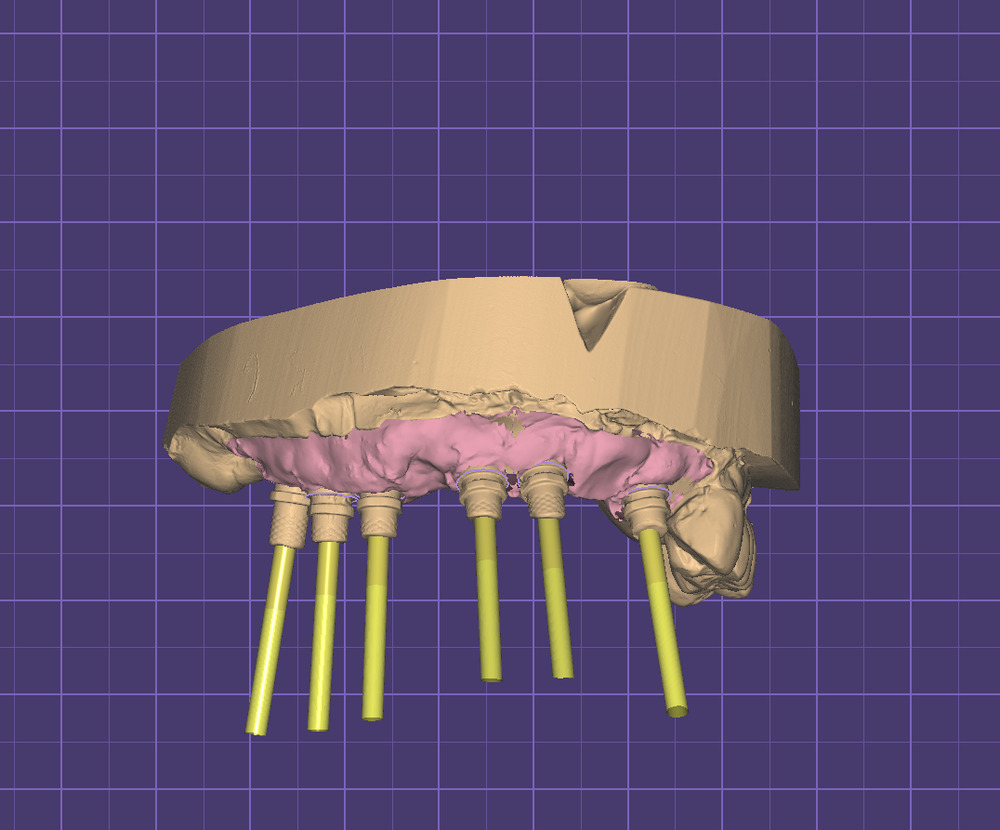
The new digital image of the working model with abutments was merged with the image of the old prosthetic restoration, which was saved in the program (Figure 11).

Within a few hours, a provisional conditionally removable restoration was made and placed in the mouth (Figure 12).

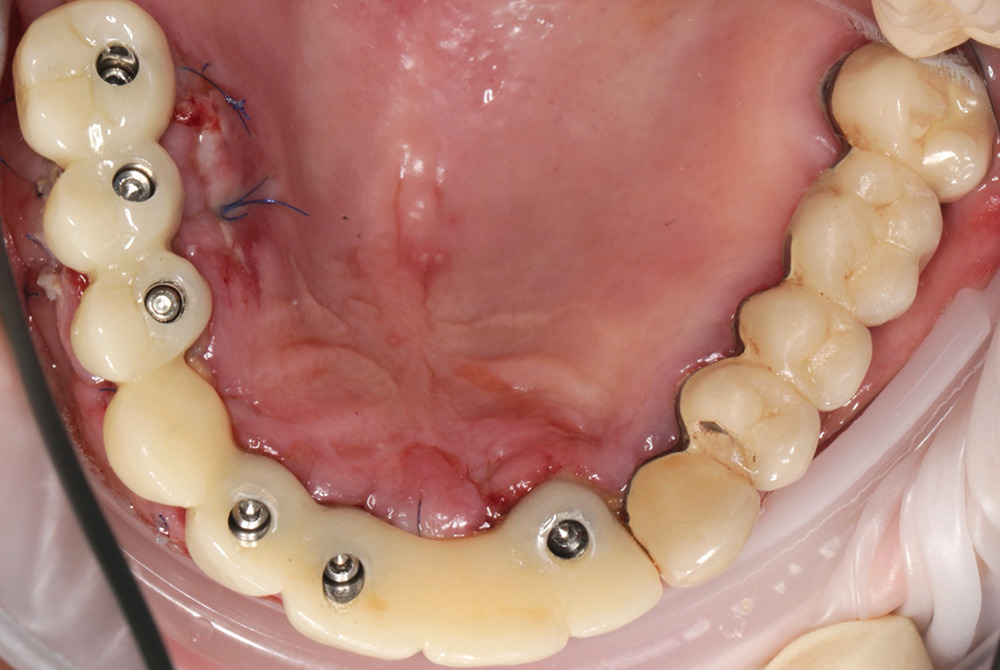
Figure. 12. Placement of a conditionally removable restoration after surgery
After 14 days, the sutures were removed and an examination was carried out (Figure 13).

The use of modern digital solutions made it possible to visualize the shape of the future prosthetic restoration, allowing for the application of immediate loading technology on implants, and to fabricate the restoration.
Conclusions
Immediate placement of a conditionally removable provisional prosthetic restoration fabricated by the analog-digital method during one-stage implantation makes it possible to speed up as well as eliminate many laboratory stages associated with human labor.
References
- Astashina N.B., Bazhin A.A., Menshikov A.E., Kazakov S.V., Bronnikov V.A. Prospects for the use of digital technologies at the stages of manufacturing removable plate prostheses. — Ural Medical Journal. — 2020; 9 (192): 72—5 (In Russ.).
- Gazhva S.I., Teterin A.I., Kushieva A.O. The use of digital technologies in prosthodontic dentistry. — Dental Forum. — 2020; 4 (79): 12—3 (In Russ.).
- Kostin K.A. Advantages of CAD-CAM digital technologies (on the example of manufacturing single ceramic restorations with the use of clinical CAD-CAM system Planmeca FIT). — International Dental Review. — 2017; 3: 12—4 (In Russ.).
- Yang Y., Yang Z., Lin W.-S., Chen L., Tan J.-G. Digital Duplication and 3D Printing for Implant Overdenture Fabrication. — J Prosthodont. — 2020 Jul 12. PMID: 32656819
- Zhao Y.J., Wang Y. Understanding chair-side digital technology for stomatology from an engineering viewpoint. — Zhonghua Kou Qiang Yi Xue Za Zhi. — 2018; 53 (4): 230—5 (In Chinese). PMID: 29690692
- Ye H.Q., Liu Y.S., Wang G.B., Wang S.M., Liu Y.S., Jia L., Sun Y.C., Zhou Y.S. Application of three-dimensional digital simulated design and implementation in esthetic rehabilitation]. — Zhonghua Kou Qiang Yi Xue Za Zhi. — 2020; 55 (10): 729—36 (In Chinese). PMID: 33045783
- Ilyichev E.A., Put V.A., Reshetov I.V., Solodkiy V.G. Surgical protocols for trans-zygomatic and angular single-stage implantation. — Proceedings of congress “Medical care for injuries in peacetime and wartime. New in organization and technology”. — Moscow, 2018. — Pp. 105—107 (In Russ.).
- Kondratjeva A.A. Treatment of patients with completely edentulous jaws using dental implants following the all-on-4 protocol. — Vestnik NovSU. — 2016; 1 (92): 77—80 (In Russ.).
- Nikitin A.A., Polupan P.V., Sipkin A.M., Nikitin D.A. Long-term results of using single-stage surgical protocol of dental implantation and one-phase dental implants. — Medical Alphabet. — 2016; 29 (292): 42—9 (In Russ.).
- Satanovsky M.A., Severinova S.K., Satanovsky A.M., Chambel-Pashaeva A.R. Our experience of orthopedic treatment of patients with non-removable designs with response to implants. — Science Diary. — 2019; 10 (34): 5 (In Russ.).
- Ershov K.A., Sevbitov A.V., Shakar‘yants A.A., Dorofeev A.E. Analysis of quality of life of elderly patients at the stage of rehabilitation with removable orthopedic designs. — Russian Journal of Dentistry. — 2017; 5: 285—7 (In Russ.).
- Grishchenkov A.S., Lyandres I.G. Laser light in the marginal gingiva aesthetics at the staged orthopedic treatment in dentistry (practical experience). — Laser Medicine. — 2019; 23 (4): 45—49 (In Russ.).
- Koshkin V.V., Maslennikov D.N., Salnikov V.N., Salnikov N.V., Simonov D.S. Rehabilitation of patients with complete absence of teeth using dental implants. — Bulletin of Medical Internet Conferences. — 2017; 1: 395 (In Russ.).
- Kondrat'eva A.A. Treatment of patients with fully edentulous jaws using Nobel dental implants following the Nobel-guide surgical template. — Vestnik NovSU. — 2017; 3 (101): 87—90 (In Russ.).
- Tavazzi E., Bergsland N., Cattaneo D., Gervasoni E., Laganà M.M., Dipasquale O., Grosso C., Saibene F.L., Baglio F., Rovaris M. Effects of motor rehabilitation on mobility and brain plasticity in multiple sclerosis: a structural and functional MRI study. — J Neurol. — 2018; 265 (6): 1393—401. PMID: 29627940
- Rubnikovich S.P., Grishchenkov A.S. Psychological profile of dental patients in prosthetics with traditional full removable dentures and removable dentures based on dental implants. — Dentist (Minsk). — 2019; 1 (32): 71—6 (In Russ.).
- Chesnokov V.A., Chesnokova M.G., Nesterova K.I., Musienko A.I. Hygienic assessment of the oral cavity in individuals with excess body mass index during orthopedic rehabilitation with removable dentures. — Parodontologiya. — 2019; 3: 269—73 (In Russ.).
- Rubnikovich S.P., Agievcev A.D. Prosthetics for patients with removable dentures based on dental implants using digital technology. — Dentist. Minsk. — 2019; 1 (32): 60—5 (In Russ.).
- Lutskaya I.K., Novak N.V. Stabilization of teeth in the clinic of aesthetic dentistry. — Sovremennaya stomatologiya. — 2016; 1 (62): 27—31 (In Russ.).
- Martínez M.F.E., López S.R., Fontela J.V., García S.O., Quevedo M.M. A New Technique for Direct Fabrication of Fiber-Reinforced Composite Bridge: A Long-Term Clinical Observation. — Dent J (Basel). — 2020; 8 (2): 48. PMID: 32397587
- Kim H., Song M.-J., Shin S.-J., Lee Y., Park J.-W. Esthetic rehabilitation of single anterior edentulous space using fiber-reinforced composite. — Restor Dent Endod. — 2014; 39 (3): 220—5. PMID: 25110647
- Ahmed K.E., Li K.Y., Murray C.A. Longevity of fiber-reinforced composite fixed partial dentures (FRC FPD)-Systematic review. — J Dent. — 2017; 61: 1—11. PMID: 28356189
- Izgi A.D., Eskimez S., Kale E., Değer Y. Directly fabricated inlay-retained glass- and polyethylene fiber-reinforced composite fixed dental prostheses in posterior single missing teeth: A short-term clinical observation. — The Journal of Adhesive Dentistry. — 2011; 13(4): 383—391. DOI: 10.3290/j.jad.a19470
- Pankratz V., Zimmer S., Marković L. Anterior fiber-reinforced ribbon composite resin bridge—A case report. — Clin Case Rep. — 2018; 6 (10): 1941—6. PMID: 30349703
- Tacir I.H., Dirihan R.S., Polat Z.S., Salman G.Ö., Vallittu P., Lassila L., Ayna E. Comparison of load-bearing capacities of 3-unit fiber-reinforced composite adhesive bridges with different framework designs. — Med Sci Monit. — 2018; 24: 4440—8. PMID: 29950555
- Kharalampos M., Put V.A., Tarasenko S.V., Reshetov I.V. Comprehensive patient rehabilitation while performing immediate dental implant placement with the use of information-wave therapy (literature overview). — Journal of Advanced Pharmacy Education and Research. — 2020; 4: 11—4. https://japer.in
- Put V.A., Tarasenko S.V., Reshetov I.V., Kharalampos M. Integrated rehabilitation of patients at the conduct of one-term dental implantation using information-wave therapy. — Russian Bulletin of Dental Implantology. — 2019; 3—4 (45—46): 90—6 (In Russ.).
- Pigozzo M.N., da Costa T.R., Sesma N., Laganá D.C. Immediate versus early loading of single dental implants: A systematic review and meta-analysis. — J Prosthet Dent. — 2018; 120 (1): 25—34. PMID: 29703670
- Bohluli B., Keyhan S.O., Cheshmi B., Ward C. Intraoperative dental implant complications. — In: Bagheri S.C., Khan H.A., Stevens M.R. (eds.) Complex dental implant complications. — Springer, 2020. — Pp. 29—46. DOI: 10.1007/978—3-030—47012—8_3
- Dobrzański L.B., Achtelik-Franczak A., Dobrzańska J., Dobrzański L.A. The digitisation for the immediate dental implantation of incisors with immediate individual prosthetic restoration. — Journal of Achievements in Materials and Manufacturing Engineering. — 2019; 97 (2): 57—68. DOI: 10.5604/01.3001.0013.8541










