DOI:
10.37988/1811-153X_2021_1_102Digital diagnostics and planning of orthodontic treatment with cortical ancorage
Downloads
Abstract
Orthodontic treatment of adult patients demands fundamentally new approaches to planning and realization due to the specificity of bone remodeling and necessity of orthopedic stability as the rehabilitation result in this group of patients.Material and methods.
412 computer tomograms and anthropometric data were examined. Correlation between upper jaw and upper dental arch constriction was found out due to the molar torque position definition. 20 patients orthodontic treatment results using individual palatal distractors with bone anchorage was analyzed.
Results.
1. Frequency of upper constriction relatively individual norm was 73%. 2. Frequency of upper constriction relatively lower jaw size was 95%. 3. Upper dental arch constriction was in bicuspid area I deg. — 15.7%, II deg. — 84.3%; in molar area I deg. — 84.9%, II deg. — 15.1%. 4. Upper jaw expansion using skeletal anchorage was 11.75±0.53 mm in average.
Conclusion.
Absolute anchorage helps to decrease treatment time and periodontal loading while teeth movements, which is positive for patient’s dental health and his satisfaction with treatment. Digital treatment planning is a perspective way of general dentistry and orthodontics in particular development as it provides exact and predictable result.
Key words:
bone anchorage, palatal distraction, orthodontic treatment, digital planningFor Citation
Introduction
The appealability of adult patients with complete skeletal growth for orthodontic treatment is steadily rising for several reasons. The main are — the necessity of orthodontic preparation for prosthetic treatment which importance leaves no doubt due to proved more stable and functional results of prosthodontics after previous dental and occlusal relationship normalizing; and not decreasing social requirements for person’s appearance in general and his smile in particular [5, 10, 17—19, 25, 27].
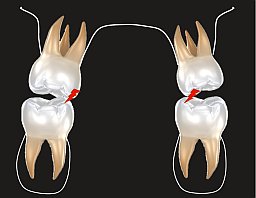
At the same time complete skeletal growth imposes a number of restrictions in standard approaches in orthodontics. Because of this the relevance of dental and skeletal parameters definition in order to evaluate those restrictions is impossible to overestimate. According to modern literature data the skeletal upper jaw constriction make up 10—32% among adult orthodontic patients [3, 4, 7, 8, 11, 14]. There is literature data indicating the presence of side effects of palatal expansion — dento-alveolar changes — increasing of vestibular upper molars inclination [2, 9, 20, 29]. Given that the narrowing of the base of the upper jaw is usually already accompanied by excessive inclination of the lateral group of teeth as a result of a lack of space, the presence of such a side effect becomes critical in most cases. "Hanging" molar palatal cusps leads to the deformation of the Wilson curve, the appearance of undesirable occlusal contacts and the absence of stable occlusion (Fig. 1).
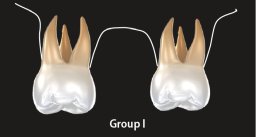
Another facet of the treatment of patients with complete skeletal growth is the features of bone remodeling under load. Expansion at the dentoalveolar level is possible only if there is a sufficient amount of alveolar bone [1, 12, 30]. The existing deficit of the base width significantly limits the vestibular movements of the teeth. Traditional distractors with a dental support develop an orthopedic force of more than 350 g/cm2 when activated, which results in resorption of not only the alveolar bone, but also the cortical plate. Due to the absence of subcostal apposition while loading in adult patients, the probability of periodontal complications of this technique increases sharply. In the case of pre-existing periodontal pathology, which is expressed in non-inflammatory resorption of the external cortical plate, further vestibular movement of the teeth is contraindicated and the question arises about the corpus dilatation of the upper jaw (Fig. 2).
One of the approaches to orthodontic treatment in such cases is the use of the SARPE (Surgical Assisted Rapid Palatal Expansion) technique — rapid palatal expansion with a surgical aid. This technique allows you to obtain an effective corpus extension of the upper jaw with the absence of undesirable periodontal effects. The disadvantages of the method include the fact that it is a full-fledged surgical intervention that requires hospital conditions, general anesthesia, and a recovery period after the intervention.
Thus, it becomes obvious that a promising direction of practical orthodontics is the search for a method for correcting the transversal deficit of the upper jaw and restoring the coordination of the dentition in adult patients with complete skeletal growth and the use of minimally invasive techniques. And one of these techniques, actively developing at the present time, is the use of cortical support for palatal expansion.
The aim of the work was to determine an effective approach to the planning and implementation of orthodontic treatment of adult patients with maxillary constriction. To achieve this goal, the following tasks are formulated:
- Conduct a cohort retrospective study of the diagnostic data of patients prior to treatment to determine the degree of narrowing of the dentition.
- To determine the correlation between the narrowing of the apical base and the dentition in patients with dental anomalies.
- Based on the obtained diagnostic data, determine the optimal method of hardware expansion and its place in the general algorithm of orthodontic treatment.
Materials and methods
We studied 412 CBCT of patients selected by random sampling who applied for orthodontic treatment from February 2017 to the end of 2019. We determined the presence and magnitude of constriction of the upper jaw along the outer cortical plate relative to the individual norm, as well as relative to the lower jaw (transversal mismatch of the jaws). We studied the data of anthropometry of 412 patients-measuring the width of the dentition using the A. Pont method. The size of the space deficit in the dentition was determined using the methods of measuring the length of the lateral segments by the method of H.G. Gerlach and using the VTO analysis by the method of R.P. McLaughlin, J.C. Bennett. Indications for hardware expansion of the upper jaw (the presence of narrowing at the skeletal level, the presence of a transversal mismatch) and for distalization of the lateral segments (lack of space in the dentition without a transversal mismatch) were determined. The correlation between the degree of narrowing of the base of the upper jaw and the dentition in degrees was determined in order to determine the axial position of the lateral group of teeth of the upper jaw. The analysis of the treatment of 20 patients using individual distractors and distalizers manufactured according to the Fit-Free™ method was carried out.
Results
The frequency of narrowing of the apical base of the upper jaw relative to the individual norm was 73% of the number of all studied cases. The frequency of narrowing of the upper jaw relative to the lower jaw was 95% of all the cases studied, thus, in the presented sample, the vast majority of patients had a transversal discrepancy between the width of the bases of the upper and lower jaw. The narrowing of the upper dentition was: the areas of premolars of the first degree — 15.7% of cases, of the second degree — 84.3% of cases; in the area of molars-of the first degree — 84.9% of cases, of the second degree — 15.1% of cases.
As part of the study of the possibilities of conservative expansion of the upper jaw and distalization of the lateral segments using cortical support, the following results were obtained. The expansion was performed in the presence of a transversal mismatch of the jaws and a lack of space in the dentition, combined with a narrowing of the upper jaw. Distalization of the lateral segments was performed in the presence of a lack of space in the dentition, but in the absence of a transversal discrepancy and indications for the expansion of the upper jaw. The expansion of the upper jaw at the skeletal level was on average 11.75±0.53 mm according to computer tomogram measurements. The value of distalization of the lateral segments of the upper jaw averaged 9.35±0.35 mm according to computer tomogram measurements.
Discussion
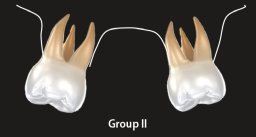
According to the results of the comparison of the anthropometric data, all patients were divided into three groups:
- uniform narrowing of the apical base and dentition — 11.3% of cases;
- apical basis of the entire dentition — 60.8% of cases;
- dentition of the already apical base — 8.96% of the total number of studied case histories (Fig. 3).
Thus, it becomes obvious that the vast majority of patients (groups I and II) have either a corpus constriction of the upper jaw and the upper dentition, or a narrowing of the base of the jaw with a vestibular slope of the lateral segments.
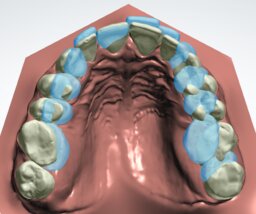
Such patients are shown to plan orthodontic treatment with the use of additional methods, for example, such as the expansion of the upper jaw with the use of cortical support (Fig. 4), and the search for a method for correcting the transversal deficit of the upper jaw and restoring the coordination of the dentition in adult patients with complete skeletal growth and the use of minimally invasive techniques is a promising direction of practical orthodontics.
From May 2019 to the present, we have been involved in the development and active use of Fit-Free technology-planning and manufacturing of orthodontic devices with cortical support and templates for their simultaneous installation. To create the device, a full digital protocol is used, which allows you to get the maximum accuracy. Intraoral scanning is performed and STL files are exported to the digital laboratory.
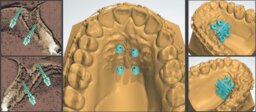
By combining CT scans and scans of models or dental rows of the patient, the optimal location of the palatal screws is determined, taking into account the anatomy of the upper jaw. Virtual installation of the screws in the safe area is performed, taking into account the route of introduction of the device, the axial load when it is activated, and the thickness of the mucosa. In the simulation program, an individual device is designed, taking into account the position of the previously designed cortical support. In the application for any mobile device, the doctor can view the entire case of patient planning, from the installation of screws to the design of the device and edit the modeling process at any stage (Fig. 5).
After the construction is completed, the template for installing the screws and the machine itself are sent for 3D printing. The template is made of polymer; the device is made of metal. This manufacturing algorithm allows you to install the device and the support screws in one visit. First, the palatal screws are installed according to the template, with the help of a nozzle on the corner tip, the sleeve of which enters the holes of the template, not allowing the screw to deviate from the specified trajectory. Then the device is installed and fixed with fastening screws.
Depending on the treatment plan, a bracket system can also be installed at the same appointment. The preliminary digital set-up, on which the superimposition is performed (blue indicates the initial position of the teeth, white-the final one), allows you to calculate the volume of the required expansion by conducting comparative measurements with an accuracy of up to thousandths of mm (with the possibility of visualizing the measurement results in the images), and to determine the indications for hardware expansion using a cortical support (Fig. 6).
With full activation of the expanding and distalizing screws in the mode of activation of the middle expansion (1/2 turn of the screw per week), it is possible to obtain an expansion of 11.75±0.53 mm with the opening of the palatal suture by moving the lateral segments in 24 weeks and distalization by 9.35±0.35 mm without side effects in the form of vestibular tilt of the teeth and destruction of the external cortical plate and periodontal overload (Fig. 7), which confirms the literature data with similar conclusions [13, 22—24, 28].
Conclusions
The predominance of narrowing of the apical bases over narrowing of the dentition indicates a high prevalence of dentoalveolar anomalies associated with excessive vestibular tilt of the teeth, which, in turn, leads to disturbances in the distribution of occlusal load and a decrease in the stability of the occlusion as a whole. Such patients are shown to plan orthodontic treatment using additional methods, such as extension using cortical support. The digital protocol of planning and modeling of devices for expansion allows you to increase the accuracy of manufacturing individual devices, reduce the time of installation and activation of equipment to 2 visits (1st — intraoral scanning and diagnostic examination; 2nd — installation of equipment), as well as determine the required volume of tooth movement with high accuracy.
Figures
References
- Almuratova A.S. Gingival recession. — Medicine and Ecology. — 2018; 1 (86): 15—22 (In Russ.).
- Al-Jafari A.R., Uliyanovskaya S.A., Davydov A.B. Skeletal and dental changes 1 month after maxillary expansion. — Morphology. — 2020; 157 (2-3): 16—7 (In Russ.).
- Arsenina O.I., Popova N.V., Mahortova P.I., Gairbekova L.A. A comprehensive diagnostics and treatment of patients with narrowing and deformities of the upper jaw. — Clinical Dentistry (Moscow). — 2019; 1(89): 51—7 (In Russ.).
- Domenuk D.A., Vedeshina E.G., Dmitrienko S.V. Main anatomic landmarks of detecting match between teeth size and dental arch parameters. — Pediatric Dentistry and Prophylaxis. — 2015; 4 (55): 45—50 (In Russ.).
- Maksimovskaya L.N., Fokina N.M., Ivanova E.P., Dudnik E.N., Stepanov P.S. Some aspects of occlusal disorders: definition, clinical objectification. — Medical alphabet. — 2015; 3 (13): 39—42 (In Russ.).
- Mamedova L.A., Efimovich O.I., Siukaeva T.N. Value of occlusal forces on dental health. — Medical alphabet. — 2016; 18 (281): 41—4 (In Russ.).
- Makhortova P.I., Arsenina O.I., Gaibekova K.A. Contemporary methods of maxilla expansion. — Proceedings of “Innovations in national economy industries as a solution factor of modern social and economic problems” conference. — Moscow, 2017. — Pp. 305—312 (In Russ.).
- Nikolaev A.V., Andreishchev A.R., Kutukova S.I. comparative biomechanical study of surgically assisted rapid palatal expansion with tooth-borne and bone-borne expanders. — Stomatology. — 2017; 96 (5): 48—55 (In Russ.).
- Popova N.V., Arsenina O.I., Makhortova P.I. Efficiency of orthodontic treatment in combination with surgically assisted rapid palatal expansion. — Stomatology. — 2019; 98 (4): 71—9 (In Russ.).
- Rotar R.B., Volchek D.A., Ospanova G.B. Analysis of TADS and TPA efficiency in orthodontic ancorage. — Orthodontics. — 2017; 3 (79): 87 (In Russ.).
- Ryahovskiy A.N., Boitsova E.A. 3D-analysis of temporomandibular joint and occlusal relations based on computer virtual simulation. — Stomatology. — 2020; 99 (2): 97—104 (In Russ.).
- Barrabé A., Meyer C., Bonomi H., Weber E., Sigaux N., Louvrier A. Surgically assisted rapid palatal expansion in class III malocclusion: Our experience. — J Stomatol Oral Maxillofac Surg. — 2018; 119 (5): 384—38. PMID: 29753777
- Brunetto D.P., Sant’Anna E.F., Machado A.W., Moon W. Non-surgical treatment of transverse deficiency in adults using Microimplant-assisted Rapid Palatal Expansion (MARPE). — Dental Press J Orthod. — 2017; 22 (1): 110—25. PMID: 28444019
- Cantarella D., Dominguez-Mompell R., Mallya S.M., Moschik C., Pan H.C., Miller J., Moon W. Changes in the midpalatal and pterygopalatine sutures induced by micro-implant-supported skeletal expander, analyzed with a novel 3D method based on CBCT imaging. — Prog Orthod. — 2017; 18 (1): 34. PMID: 29090368
- Carvalho P.H.A., Moura L.B., Trento G.S., Holzinger D., Gabrielli M.A.C., Gabrielli M.F.R., Filho V.A.P. Surgically assisted rapid maxillary expansion: a systematic review of complications. — Int J Oral Maxillofac Surg. — 2020; 49 (3): 325—32. PMID: 31500954
- Charavet C., Lambert F. [A multidisciplinary approach for accelerated orthodontics]. — Rev Med Liege. — 2020; 75 (5—6): 452—6 (In French). PMID: 32496696
- Chow L., Goonewardene M.S., Cook R., Firth M.J. Adult orthodontic retreatment: A survey of patient profiles and original treatment failings. — Am J Orthod Dentofacial Orthop. — 2020; 158 (3): 371—82. PMID: 32709577
- Flores-Mir C., Brandelli J., Pacheco-Pereira C. Patient satisfaction and quality of life status after 2 treatment modalities: Invisalign and conventional fixed appliances. — Am J Orthod Dentofacial Orthop. — 2018; 154 (5): 639—44. PMID: 30384934
- Jheon A.H., Oberoi S., Solem R.C., Kapila S. Moving towards precision orthodontics: An evolving paradigm shift in the planning and delivery of customized orthodontic therapy. — Orthod Craniofac Res. — 2017; 20 Suppl 1: 106—13. PMID: 28643930
- Jiang L., Zheng Y., Li N., Chen X., Lu Z., Tong H., Yin N., Song T. Relapse rate after surgical treatment of maxillary hypoplasia in non-growing cleft patients: a systematic review and meta-analysis. — Int J Oral Maxillofac Surg. — 2020; 49 (4): 421—31. PMID: 31526673
- Krishnaswamy N.R., Varghese B.T., Ahmed K.S., Bharadwaj R., Devi V.R.S. Treatment of a unilateral complete lingual crossbite in an adult with skeletal anchorage assisted orthodontics. — J Orthod. — 2016; 43 (3): 228—36. PMID: 26777996
- Lim H.-M., Park Y.-C., Lee K.-J., Kim K.-H., Choi Y.J. Stability of dental, alveolar, and skeletal changes after miniscrew-assisted rapid palatal expansion. — Korean J Orthod. — 2017; 47 (5): 313—22. PMID: 28861393
- Mohamed R.N., Basha S., Al-Thomali Y. Maxillary molar distalization with miniscrew-supported appliances in class II malocclusion: A systematic review. — Angle Orthod. — 2018; 88 (4): 494—502. PMID: 29664335
- Papakostopoulou M., Migliorati M., Calzolari C., Gallo F., Drago S., Biavati A.S. Patients’ expectations assessment in orthodontic treatment: findings from a questionnaire survey. — Minerva Stomatol. — 2016; 65 (6): 343—52. PMID: 27362809
- Park J.J., Park Y.-C., Lee K.-J., Cha J.-Y., Tahk J.H., Choi Y.J. Skeletal and dentoalveolar changes after miniscrew-assisted rapid palatal expansion in young adults: A cone-beam computed tomography study. — Korean J Orthod. — 2017; 47 (2): 77—86. PMID: 28337417
- Sabri R., Aboujaoude N. [Adult orthodontics for a better prosthesis]. — Orthod Fr. — 2018; 89 (2): 145—56 (In French). PMID: 30040614
- Soheilifar S., Mohebi S., Ameli N. Maxillary molar distalization using conventional versus skeletal anchorage devices: A systematic review and meta-analysis. — Int Orthod. — 2019; 17 (3): 415—24. PMID: 31255550
- Strohl A.M., Vitkus L. Surgical orthodontics. — Curr Opin Otolaryngol Head Neck Surg. — 2017; 25 (4): 332—6. PMID: 28538022
- Suzuki H., Moon W., Previdente L.H., Suzuki S.S., Garcez A.S., Consolaro A. Miniscrew-assisted rapid palatal expander (MARPE): the quest for pure orthopedic movement. — Dental Press J Orthod. — 2016; 21 (4): 17—23. PMID: 27653260
- Wehrbein H., Göllner P. Skeletal anchorage in orthodontics—basics and clinical application. — J Orofac Orthop. — 2007; 68 (6): 443—61. PMID: 18034286