DOI:
10.37988/1811-153X_2021_1_42Early pathognomonic signs of multiple Kaposi's sarcoma on oral mucosa, especially in mucocutaneous lesion
Downloads
Abstract
Kaposi's sarcoma (KS) on oral mucosa is an important indicator of probable HIV- infections.Materials and methods.
15 patients with KS were under observation; of which 7 were with early manifestations of KS on oral mucosa (5 were with HIV-associated KS, 2 — with idiopathic KS). All patients were examined for HIV. Diagnosis of KS is histologically verified.
Results.
Early manifestations of KS on oral mucosa are combined with analogical rashes on an open areas of the skin in large majority of patients (64—100%, p=0,05). It is the unified mucocutaneous syndrome in KS. Early manifestations of KS only on oral mucosa develop rather rare. Early pathognomonic signs of HIV-associated KS and idiopathic KS may be clinical similar — on oral mucosa and on the skin. These signs are presented in “classic” triad [M.Kaposi]: multiple, hemorrhagic, “pigmented” (dark-violet, dark-purple, brownish-lilac) spots, plaques.
Conclusion.
Recognition of mucocutaneous syndrome improves the information of clinical data. Serological HIV-test should be prescribed without waiting for histological confirmation of SK.
Key words:
Kaposi's sarcoma, oral mucosa, HIV, mucocutaneous syndromeFor Citation
Introduction
The HIV infection epidemiological situation in the world and in Russia could be characterized as a pandemic, still remains unstable, and the identification of HIV-infected patients is relevant [1, 2]. Kaposi's sarcoma (syn.: Kaposi's angiosarcoma) can serve as a clinically important indicator of probable HIV infection [3]. Kaposi's sarcoma (KS) is several thousand times more common in AIDS patients (and affects about a third of them) than in the general population [4, 5]. The oral mucosa (usually on the palate or on the gums) is affected by HIV-associated KS in 22—50% of patients [4—6]. KS on the oral mucosa is often combined with a skin KS manifestation, which is observed in more than 95% of cases [6]. Morphological differences between idiopathic KS and KS in AIDS have not yet been found [5]. The KS etiology is associated with human herpesvirus type 8 (HHV—8) [1, 4]. KS develops from the blood capillaries endothelium (venous and arterial) and small lymphatic vessels (blood/lymphatic microvasculature) [4]. The color of hemorrhagic spots and plaques varies from dark purple to purplish-purple, the hue depends of the venous and arterial capillaries damage degree. Due to the hemosiderin early deposition, a brown hue is possible [7, 8]. In case of the lymphatic vessels involving in damage process, tissue edema may occur. Subjective feelings are often absent or insignificant. The rash elements at the disease early stage do not rise, but plaques, bumps, and tumors gradually form. There is any localization of multiple KS on the mucous membranes and on the skin. The KS clinical features are briefly defined by the signs triad: “multiple, hemorrhagic, pigmented Pigmentsarkom” (M. Kaposi, 1872) [9, 10]. These signs, described for idiopathic, “classical” KS, also refer to HIV-associated KS [11, 12]. At the same time, it seems appropriate to consider the early HIV-associated KS clinical signs on the oral mucosa, especially in multiple — usually mucocutaneous affect.
The research objectives: 1) to consider the HIV-associated KS early clinical signs on the oral mucosa, especially in multiple-usually mucocutaneous affect; 2) to evaluate the KS signs "classic" triad' informative value and pathognomonicity (M. Kaposi) — in relation to the oral
Materials and methods
Into research were included 15 patients with KS: 7 men and 8 women, aged from 23 to 81 years. All patients were examined for HIV infection at the Regional Skin and Venereal Clinic (RSVC) and consulted at the AIDS Prevention Center-with a blood test for HIV using the immunoblot method. The KS diagnosis was confirmed histologically in the Regional Oncological Clinic. Early KS manifestations on the oral mucosa were detected in 7 patients: 5 with HIV-associated KS and 2 with idiopathic (“classical”) KS In 8 patients, KS manifestations were observed only on the skin (comparison group).
The statistical processing method is to determine the cases frequency confidence limits, as a percentage at p=0.05, using special tables for small samples [13]. The probability of error (p=0.05) may be ±5%.
Results
The early KS manifestations on the oral mucosa were detected in 7 out of 15 patients with KS (23—61%, with p=0.05): both in patients with idiopathic KS (Figure 1-a) and HIV-associated KS (Figure 2-a). Usually, the early KS manifestations were localized on the hard palate and had the appearance of sharply limited, oblong spots (parallel to the palatal suture), dark purple or purplish-purple, without subjective sensations. The KS manifestations on the oral mucosa should be differentiated from enanthema in secondary syphilis [14]. Subjective feelings are not typical for both diseases. Palatine erythematous angina in syphilis manifests itself in the "stereotype" form, clear rich red color spots (not purple), regular round shape (and not elongated along the palatine suture). In the case of papular syphilitic angina, macerated papules are formed, which easily lose the white coating, exposing the meat-red surface. All syphilitic rashes spontaneously regress within 3 weeks (in contrast to persistent, progressive KS). It is also necessary to differentiate from red lichen planus, in which small white papules appear on the oral mucosa (usually not on the hard palate), which are arranged linearly (Koebner phenomenon, isomorphic reaction) or are grouped together to form a mesh pattern (Wickham's striae) [5].


Early KS manifestations on the oral mucosa were combined with KS manifestations on the skin (in open, visible areas) in all 7 of 7 patients (64—100%, p=0.05), both in idiopathic KS (Fig. 1b) and in HIV-associated KS (Fig. 2b, 3).
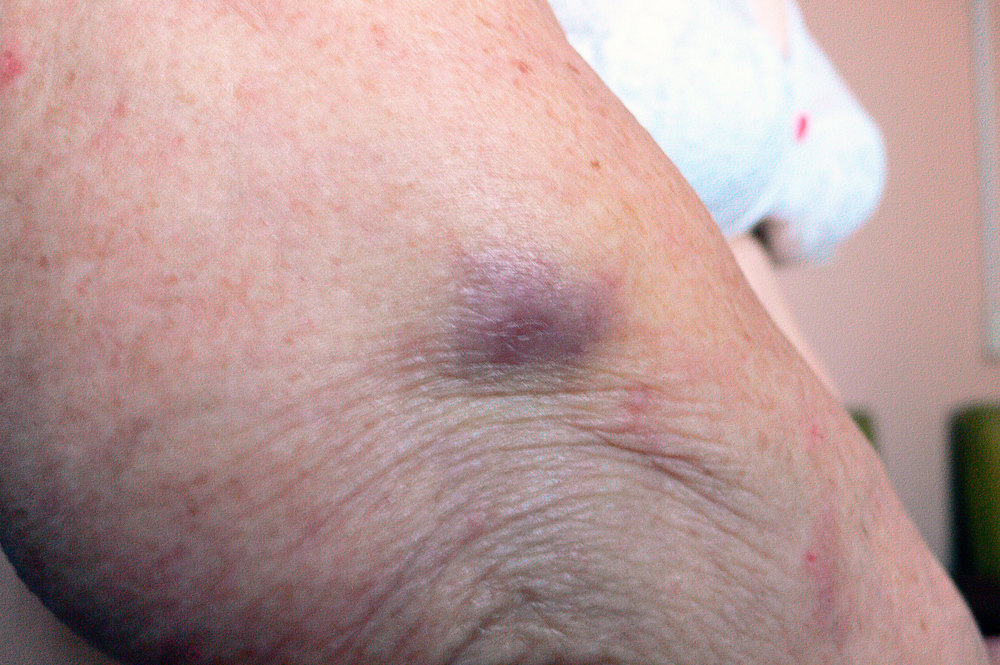

Early KS manifestations on the skin were rounded spots and plaques, which were as on the mucous membrane dark purple or purplish-purple. The "fresh" spots, which were still forming, had less clear outlines and were pinkish-purple (Fig. 2c). Gradually, the rash color becomes more saturated and dark. The patient often has rash elements at different development stages (Fig. 2-d): the "fresh" spot (under the knee) is still pinkish — purple, with indistinct borders, and the already formed plaque (above the knee) is purplish-purple, sharply defined.


The KS recognition as a single mucocutaneous syndrome significantly increases the informative value of clinical data and contributes to the early detection of patients with HIV infection. Patient A. (Fig. 3) went to the dentist for oral cavity sanitation. This patient was examined in a clinic for edematous hemorrhagic spots that appeared on it's face, similar to ”bruises”(and made face looks “asocial appearance”). There were no injuries. Data for hematological disease and for allergy were not revealed. The dentist also found purplish-purple, asymptomatic spots on the mucous membrane of the hard palate. Blood tests for syphilis and HIV were scheduled. The test is positive for HIV. The patient was sent to the AIDS Prevention Center and for consultation in an oncological clinic. The diagnosis is Kaposi's sarcoma (confirmed histologically). Anti-retroviral therapy has being carried out.

Discussion
The KS early signs on the oral mucosa are combined with similar multiple KS manifestations on the skin in 64—100% (p=0.05). The combined affects high frequency (tends to 100%) allows to consider this phenomenon as a mucocutaneous syndrome — KS characteristic. This syndrome can serve as an additional diagnostic guide that increases the clinical data informative value and responsibility, contributing to the early KS recognition.
The main KS clinical signs, presented in the "classical" triad: multiple, hemorrhagic, pigmented, relate to Kaposi's sarcoma in general (81—100%, with p=0.05; / 15 out of 15 patients/) and including KS on the oral mucosa (64—100%, p=0.05; /7 out of 7 patients/). These signs are generally pathognomonic for Kaposi's sarcoma, since they reflect the characteristic links of its pathogenesis.
- Multiple KS: numerous blood and lymphatic capillaries damage (blood/lymphatic microvasculature), from the endothelium of which tumors are formed [4].
- Hemorrhagic KS: blood capillaries dilation and overflow in the affected areas, with the appearance of hemorrhage sites at a KS early stage [8].
- "Pigmented" KS ("Pigmentsarkom") [9]. This characteristic should be considered not only in relation to early deposition of pigment (hemosiderin), but as a symbol generally distinctive KS manifestations — dark shade of a color: dark purple (stagnation of venous blood in the capillaries), deep crimson (blood stasis in the dilated arterial and venous capillaries) [8].
Conclusion
- Early clinical Kaposi's sarcoma (KS) signs on the oral mucosa are usually combined with similar rashes on the skin (in open, visible areas), which makes possible to consider this combination as a single mucocutaneous syndrome, the recognition of which increases the informative value of clinical data.
- The early KS clinical signs on the oral mucosa, as well as in general with mucocutaneous affect, fulfil to the “classic” triad: multiple, hemorrhagic, pigmented (dark purple, purplish-purple, brownish-purple) spots and plaques.
- If any KS signs are detected, it is necessary to prescribe a blood test for HIV to the patient, without waiting for the KS diagnosis histological examination and confirmation.
- The KS problem is interdisciplinary, but its solution could begin with a patient's dentist visit.
References
- Tschachler E. Kaposi's sarcoma. — In: Wolff K., Goldsmith L.A., Katz S.L. et al. (eds.) Fitzpatrick's Dermatology in General Medicine. — 7th ed. — NY: McGraw-Hill Medical, 2008. — Vol. 2, chap. 128.
- Shatohin A.I., Rabinovich I.M. Oral Kaposi angiosarcoma — the AIDS indicator and predictor. — Clinical Dentistry (Russia). — 2017; 83 (3): 36—8 (In Russ.).
- Bartlett J.G., Gallant J.E., Pham P.A. Medical Management of HIV Infection. — USA: Knowledge Source Solutions. — Chapter 7.
- Zavadsky V.N. Early pretumor symptoms of Kaposi´s sarcoma. — Oncosurgery. — 2013; 5 (Special issue 1): 8 (In Russ.).
- Zavadsky V.N., Romanova N.V. Clinical signs of Kaposi's multiple sarcoma on skin and on oral mucosa: cases from practice. — Russian Journal of Clinical Dermatology and Venereology. — 2020; 19 (4): 470—475. (In Russ.).
- Zavadsky V.N. The clinical features of contagious manifestations of syphilis on oral mucosa. — Clinical Dentistry (Russia). — 2019; 4 (92): 28—31 (In Russ.).










